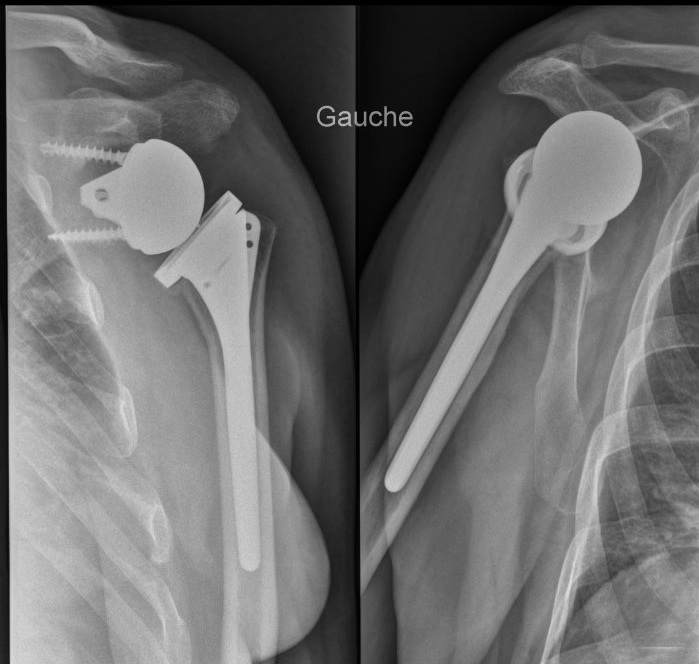
The laying of a shoulder prosthesis results in the vast majority of cases to a benefit for the patient, indolence and improvement of the function.
Sometimes unfortunately the consequences are not simple, stiffness long to recover, persistence of pain but there are also complications that can lead to reinterventions: