Sprains or dislocations (or ‘dysjunctions’) are common in sports pathology or traffic accidentology.
You will find explanations on
– the different traumatic stages which correspond to more and more severe lesions,
– indications of conservative treatment (non-surgical) and surgical treatment
– the surgical technique we have chosen
– as well as a video of a case performed under arthroscopy.
Classification
To know the anatomy of the acromioclavicular joint click here
Or to know more about clavicular osteoarthritis
During a fall on the shoulder, especially in case of direct shock, may occur acromioclavicular joint trauma whose severity may be variable.
This situation is a frequent reason for emergency or delayed consultation, with the physician using ‘stages’ of gravity that can be summarized as follows (without entering classification names …):
Stage 1:
This is a ‘simple’ sprain with distension or even partial tear of the acromioclavicular joint capsule and / or acromioclavicular ligaments (see chapter anatomy of the acromioclavicular joint)
= At the origin of a pain above the shoulder as soon as the mobilization of the arm, sometimes accompanied by a small bump painful with the pressure (effusion of blood in the articualtion or ‘hemarthrosis’). At this stage there is no deformation of the shoulder.
Stage 2:
If the trauma is more violent tearing acromioclavicular ligaments is complete with appearance of a larger hump, a touch of piano during the pressure on the hump and possibly anteroposterior mobility called ‘drawer anteroposterior’. The weight of the arm draws the shoulder down and thus causes a ‘rise’ of the clavicle, partial at this stage because of the integrity of the coraco-clavicular ligaments.
Stage 3:
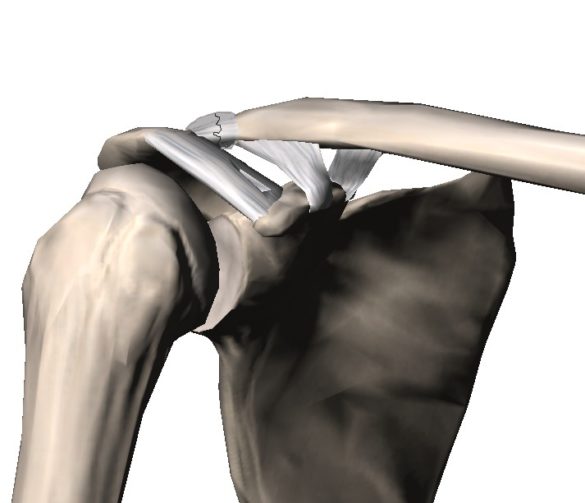
The coraco-clavicular ‘suspension’ ligaments are subsequently broken, resulting in a complete dislocation between the shoulder and the clavicle, a visible fall of the shoulder stump always due to the weight of the upper limb.
Stage 4 :
The superior muscular catechism comprising the trapezius and the deltoid (stabilizer of the AC joint) is finally injured with skin clavicle appearance and extreme instability or a very painful incarcerated clavicle.
indications
De manière consensuelle, les stades 1 et 2
Un strapping peut être mis en place afin de stabiliser au début l’articulation instable et parfois très douloureuse
Le stade 4 est chirurgical
Le stade 3
Acromioclavicular Ligamentoplasty
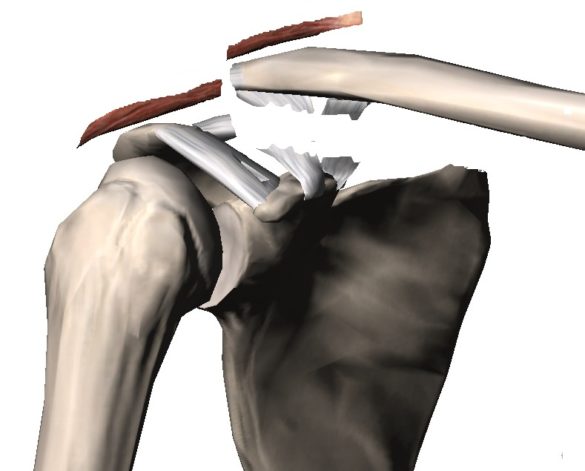
Acromioclavicular ligamentoplasty reduces acromioclavicular diastasis by reducing limb drop and reducing coraco-clavicular space.

diastasis caused by the fall of the arm
reduction of diastasis after ligamentoplasty allowing ligament healing during the first 3 weeks
In all cases, we perform an artificiform ligamentoplasty, but there are two very different types of intervention depending on the time of the trauma:
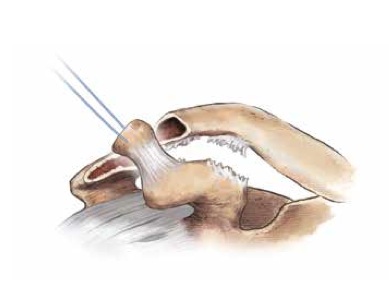
Recent or acute dysjunction (before 3 weeks): ligamentoplasty sufficient
Directed healing of coraco-calvicular ligaments is required +++
Several techniques exist to fight against the fall of the shoulder and allow healing of coraco-clavicular ligaments
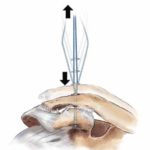
- Acromioclavicular ‘osteosynthesis’, using equipment (pins, strapping, plate) now at the same level acromion and clavicle for a limited time
- Coraco-clavicular osteosynthesis (lassoing or screwing between the clavicle and the coracoid)
- Artificial acromioclavicular ligamentoplasty (our choice), which aims to allow the healing of coraco-clavicular ligaments by fighting against acromioclavicular diastasis.
It is sometimes necessary to approach the joint in order to extricate the muscular cleft or part of the articular material, or even resect the lateral end of the clavicle to allow perfect acromioclavicular reduction.
Old or chronic dysjunctions:
a ligament replacement is essential
Beyond 3 weeks it is estimated that the broken ligaments located between the clavicle and the coracoid no longer have the ability to heal and a ligament transplant (replacement of ligaments) is essential in combination with the artificial ligament.
the same stabilization techniques can be used but obviously all healing of the coraco-clavicular ligaments is illusory
.
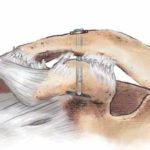
- locally use of the coracoacromial ligament, most often used in France (Waever Dunn or Cadenat technique)
- either auto see tendonous graft (clean tendon from distance or from another person).
Chronic forms: removal of a ligament graft
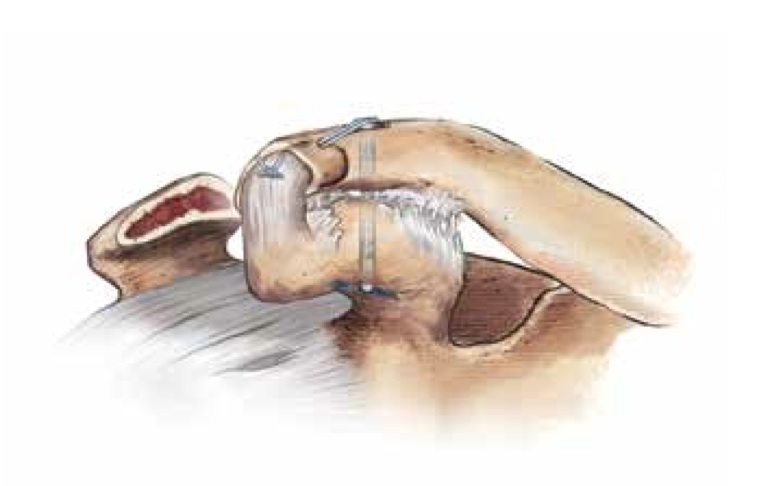
Ligamentary transplant in place (intervention by Waever and Dunn)
Acromioclavicular video
Look at an acromioclavicular ligamentoplasty under ligamentous ligamentous arthroscopy as part of a chronic dislocation in a Rugbyman!
Acromioclavicular osteoarthritis
Acromioclavicular osteoarthritis is very common, often asymptomatic but may explain acromioclavicular pain.
The causes of acromioclavicular pain are most often related to inflammation of this joint related to:
- old trauma (eg disjunction)
- joint overwork (profession and / or heavy manual activity, sports, physiotherapy of the shoulder !!)
- osteoarthritis or cartilage wear, generally corresponding to an evolution of one of the cases mentioned above,
- secondary osteoarthritis (see causes of osteoarthritis) or idiopathic osteoarthritis (no identifiable cause).
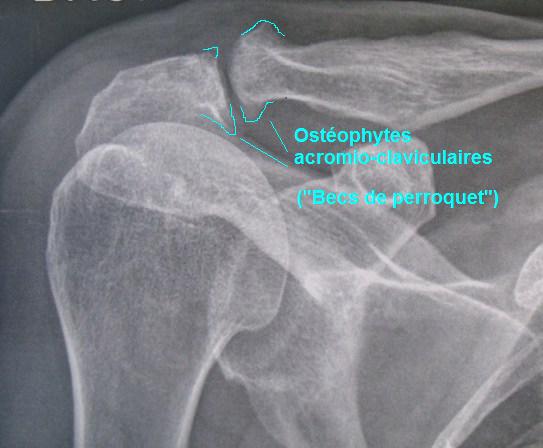
Acromioclavicular osteoarthritis responsible for a related ‘sub-acromioclavicular’ conflict
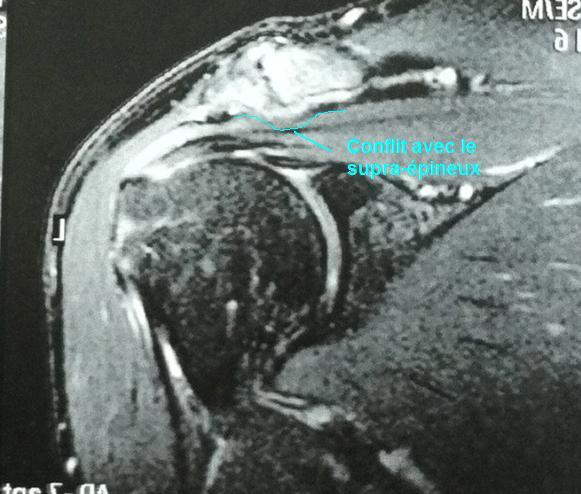
Hypersignal of an acromioclavicular joint
Two symptomatologies exist, isolated or associated:
- joint pain associated with internal inflammation of the joint that is swollen and is very sensitive during movement and pressure on the top of the shoulder
- either the deformation of this joint (articular arch or parrot beaks related to osteoarthritis) causes a conflict with the cap including the myotendinous junction of the supra-thorny located just below, then leading to sub-acromial bursitis and tendonitis of the supraspinatus. She then participates in the conflict under ‘acromioclavicular’.
Resection of the acromioclavicular joint
Treatments
The treatment is first medical, joint rest, identification of possible factors favoring and if possible eviction of them; shoulder glazing, anti-inflammatory, physiotherapy with physiotherapy etc …
If these elements are not sufficient, one or more acromioclavicular infiltrations can be performed with a mixture of local anesthesia that can test the possible relief of infiltration in real time (immediate but very fleeting action of local anesthesia).
In case of symptoms of acromial inflammation or tendonitis of the supraspinatus, refer to the chapter on tendinopathy of the cuff.
In case of failure of the medical treatment an intervention can be considered at best arthroscopy in the form of a resection of the acromioclavicular joint using a motorized bur and lower osteophytes.